



Non-surgical oncology (often called NSO) is the part of cancer care that does not involve surgery. It includes:
- Chemotherapy
- Radiotherapy
- Care for people who become unwell because of their cancer or treatment (known as acute oncology).
NSO services in our region are organised in a unique way that was agreed more than 20 years ago. However, after engaging with public, patients and professionals, this model is changing to make care safer, more reliable and as close to home as possible
Here is where you can learn more about non-surgical oncology, the improvements being developed and why the changes are needed. Read more below.

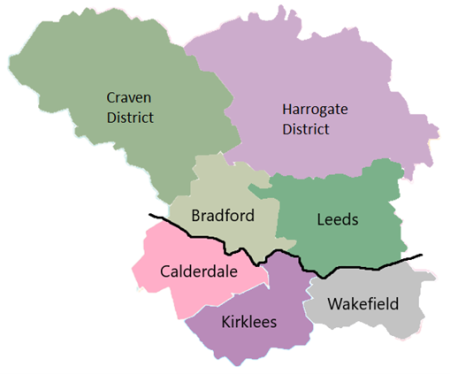
For many years, NSO services in West Yorkshire were organised differently from most of the country. Each local hospital (Cancer Unit) employed its own specialist cancer doctors to provide chemotherapy and related care for the most common cancers. Specialist treatment was provided at the Leeds Cancer Centre.
Elsewhere in England, these local services are usually provided by visiting teams from the Cancer Centre.
Over time, this way of working became difficult to maintain. Key challenges included:
- A national shortage of oncologists (specialist cancer doctors).
- Difficulty recruiting other specialist staff to some parts of West Yorkshire - for example, Advanced Care Practitioners (ACPs).
- Growing numbers of people living with cancer and needing treatment for longer.
- Pressure on acute oncology services from growing patient numbers and new treatments with side-effects that can be more complex to manage.
- High reliance on temporary staff.
These pressures made services less consistent and less resilient. Patients and staff have told us this needed to improve.

We heard from more than 1500 people across more than 20 towns and cities in West Yorkshire and Harrogate.
The key messages we heard included:
- Strong support for treatment closer to home.
- Clear expectations for safe, consistent care across all hospitals.
- The importance of making care easy to access.
A leaflet has been produced which provides more information on how public feedback was used to co-design the new delivery model. Click here to read the leaflet.
Drug Therapies
- All hospitals in West Yorkshire and Harrogate currently offering anti-cancer drug treatments will continue to do so.
- Patients will be allowed to choose to receive chemotherapy and other anti-cancer drugs outside of hospital settings, for example on mobile services or in your home supported by district nursing, where it is safe to do so.
- Patients with rarer cancers who have to travel to Leeds Cancer Centre for outpatient appointments will be offered the opportunity to have their drug treatments (like chemotherapy) from their local hospital where safe and possible to do so ie for simple treatments.
Radiation Therapies
- Patients should not experience any significant change in radiotherapy services.
- Treatments will continue to be delivered from Leeds St James’ Hospital and doctors specialising in radiotherapy will continue to travel to local hospitals to deliver outpatient clinics for common cancers. There is a separate piece of work starting with colleagues in Leeds looking at expansion of radiotherapy services in the future.
Outpatient Clinics
- Services will be re-organised into two geographies, North and South. This merges some services and creates larger clinical teams which will be more resilient and offer a more equitable level of service.
- Outpatient clinics for the most common cancers will continue to be provided from each of the six hospital trusts. The most common cancers are lung, breast, colorectal (bowel) and prostate cancer.
- Outpatient clinics for rarer cancers will continue to be delivered from the Leeds Cancer Centre only (as is the case now).
- Outpatient clinics will be delivered in a more standard and equitable way using a combination of doctors and other cancer specialists such as senior nurses and pharmacists.
- Wherever appropriate, hospitals will give patients the option to have their outpatient clinic or monitoring remotely. This could be by telephone, video conference or use of electronic monitoring tools.
Inpatient Care
- All hospitals in West Yorkshire and Harrogate with an A&E department will continue to admit and treat patients who become unwell due to side effects of treatment or their cancer becoming more advanced.
- We will consolidate our specialist beds. Specialist inpatient beds will continue to be provided at Leeds St James' and Huddersfield Royal Infirmary.
- Most patients will be seen by at their local hospital by either the A&E medical team, a specialist acute oncology nursing team or another medical specialty – for example a cancer patient with a bowel obstruction would be seen by a surgical team.
- Bradford Hospital will continue to provide care for most complications of cancer but patients requiring specialist inpatient care will be transferred to Leeds Cancer Centre. This change will be phased in once our programme funding and implementation plans are agreed (currently aiming for end of 2027)
- Wakefield Pinderfields and Dewsbury Hospitals will provide care for most complications of cancer but patients requiring specialist inpatient care will now be transferred to Huddersfield Royal Infirmary instead of to Leeds St James'. This provides for better continuity of care as it is oncologists from Huddersfield that will be responsible for the outpatient care of these patients.
- Where required, investment will be made to increase the size of acute oncology nursing teams to support patients to stay out of hospital/ have care as close to home as possible.
The consolidation of specialist inpatient care for people with cancer will free up doctors’ time for other clinical work such as outpatient clinics and to support chemotherapy
The NSO programme presented its review with recommendations for service improvements to the West Yorkshire Association of Acute Trusts (WYAAT) in Summer 2025.
WYAAT agreed that the Cancer Alliance had identified a future model for non-surgical oncology which had significant engagement support.
Priorities were identified and by January 2026, hospitals either had in place, or had agreed, funding for around 75% of the additional workforce and actions that the review identified as being necessary.
After the government published the 10‑Year Health Plan for England in July 2025, NHS leaders asked the Cancer Alliance to make sure the new NSO model aligns with national priorities.This work focussed on:
- Reviewing the NSO model against the national 10-year plan
- Assessing capacity and demand in other parts of cancer care, such as:
- Diagnostic imaging
- Surgery
- Radiotherapy
- Pathology.
This work will be submitted to the West Yorkshire Association of Acute Trusts Programme Executive in February 2026 where any future priorities for cancer care across West Yorkshire and Harrogate will be agreed

